Abstract
Introduction and methods: Myeloma is a cancer with one of the longest pathways to diagnosis. This may be due to the non-specific nature of presenting symptoms and its' relative rarity. Early diagnosis initiatives have focused on the role of the primary physician. Despite concern that patients referred to non-haematology specialists may experience long diagnostic intervals, data remain sparse on pathways within hospital care. The TEAMM trial is a double-blind, placebo controlled multicentre UK trial of supportive care, investigating levofloxacin prophylaxis for 12 weeks from diagnosis to reduce infection, versus the risk of healthcare associated infection. Data were collected from patients within 14 days of starting anti-myeloma treatment, including symptoms attributable to myeloma, visits to their primary physician, first hospital department visited for these symptoms, and first visit to a haematologist, with corresponding dates. The relationship between diagnostic time intervals and the number of CRAB (hyperCalcaemia, Renal disease, Anaemia, Bone disease) features and ISS (International Staging System) were analysed by pathway into hospital care using the chi-square test for categorical variables or Wilcoxon/Kruskal-Wallis test for continuous variables as appropriate.
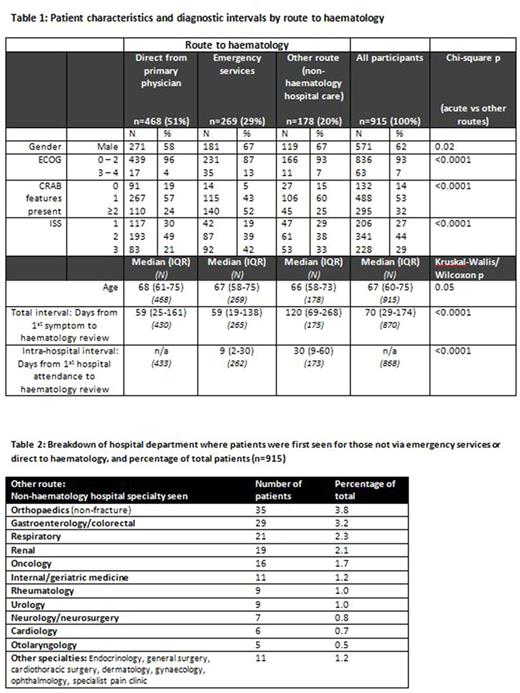
Results: Diagnostic pathway data were available for 915 patients. Table 1 presents baseline factors and diagnostic time intervals by the route to haematology. The largest group were those referred directly to haematology by their primary physician (n=468, 51%). 269 patients (29%) were 'acute' whose first hospital encounter was via the emergency services, although they were not necessarily diagnosed consequent upon the visit.178 patients (20%) were first referred to other departments. These patients experienced a longer diagnostic pathway (median 120d=days) than those first presenting via haematology clinics (median 59d) or emergency services (median 59d). A median of 30d intra-hospital delay contributed to this longer pathway. Table 2 lists the departments first visited. Two or more CRAB features were commonest in the 'acute' patients compared to the 'haematology direct' or 'other route' patients (52% vs 24% and 25%, p<0.0001). Patients presenting via other routes had a CRAB profile similar to that of the patients referred directly to haematology and significantly less severe than the acute patients (p<0.0001). Acute pathway patients were more likely to be ISS stage 3 compared to patients who entered directly to haematology, or via other routes (42% vs 21% and 29%, p<0.0001).
Discussion : The 20% of patients who entered hospital care via 'other routes' have previously been inaccessible to analysis possibly because myeloma patients are median age >70 with frequent comorbidities, making registry data difficult to interpret. Recognising these unusual protracted paths to diagnosis may provide an opportunity for healthcare improvement. Our total diagnostic time intervals were shorter than previously reported in the UK. Our endpoint was the first visit to a haematologist ie prior to the date of histological diagnosis as used in previous studies. Patient recall for events may also underestimate the earliest date of symptom onset. Total diagnostic times may overall be longer than our figures but the subgroup comparisons remain valid.
CRAB features were more common in 'acute' patients possibly reflecting more aggressive disease. The longer path to diagnosis in 'other route' patients may reflect a more indolent disease which is less easily recognised. The similarity between the CRAB profile of these and the haematology direct group versus the sicker acute patients suggests this may be the case but does not rule out missed healthcare opportunities. The relation between diagnostic time intervals and CRAB features needs to be explored further.
Conclusion: Emergency patients had more CRAB features and higher ISS and PS (performance status) than other groups. First presentation via emergency services was common (29%), even in a relatively good PS group of trial patients. 20% of patients presented via non-haematological non-emergency specialities and experienced a longer time to diagnosis, and yet despite this they had a broadly similar CRAB profile to the haematology direct patients, who had been seen more promptly. Diagnostic pathways may reflect tumour biology and need further exploration.
Bowcock: Celgene: Other: Educational support; Amgen: Honoraria; Takeda: Other: educational support. Yong: Amgen: Honoraria, Research Funding; Janssen: Honoraria, Research Funding. Drayson: Abingdon Health: Equity Ownership, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.